Dental Pulp
The dental pulp (pulpa dentis) lies in the pulp cavity and in the dentinal root canals inside the tooth. This cavity is very large in young people but later becomes progressively narrower as dentin production continues. The pulp is made up of jelly-type connective tissue that contains blood vessels, lymph, and nerve endings. The pulp is generally referred to as the "nerve" of the tooth.
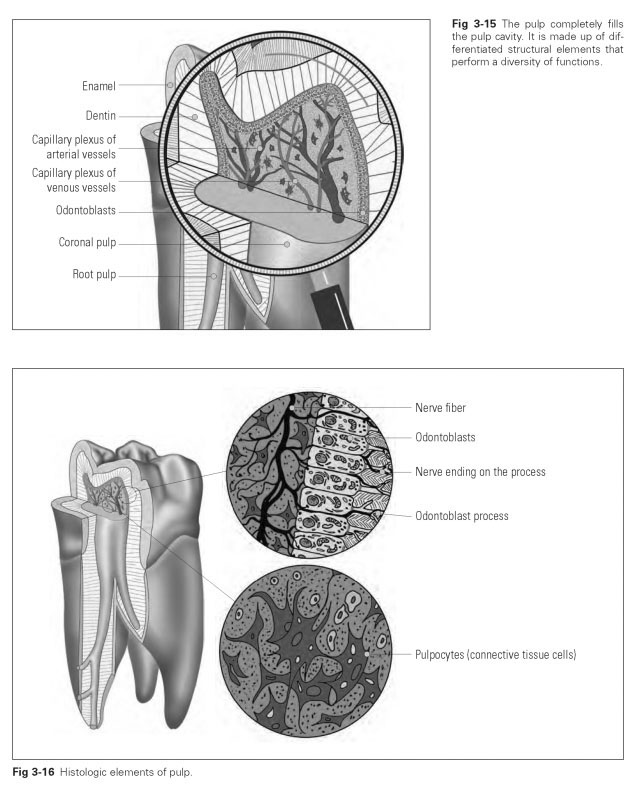
The pulp cavity is the chamber that is filled with pulp (Fig 3-15). It is subdivided into the coronal cavity and root canals. The pulp cavity of the crown follows the shape of the tooth in such a way that the pulpal horns lie under the incisal edges and tips of the cusps. The root canals generally end in an apical foramen, but they often have several canals and holes in the apical area and open into the periodontal gap. The pulp cavity and root canals become increasingly narrow as dentin synthesis progresses; the pulp gets progressively smaller, and some root canals may even grow to the point of closure.
The pulp is surrounded by a layer of odontoblasts whose processes extend into the dentin and pulp (Fig 3-16). The pulp is packed with blood and lymph vessels that enter through the apical foramina and form a dense network of vessels. Looped branches extend into the odontoblast layer. Nerve fibers also enter the pulp cavities with these vessels through the foramina. The nerve fibers pass into the coronal pulp almost without branching, where they fan out broadly. They are mostly involved in efferent nerve conduction to register pain. Terminal branches reach the odontoblasts and from there enter the dentinal tubules. Impulses that reach the odontoblast processes are thus transmitted to the free nerve endings.
Pulp tissue comprises 25% organic constituents and 75% water and performs its functions under high tissue pressure. It is a loose connective tissue that is packed with fibrils, nerves, and vessels. It develops from the dental papilla. During the formation of dentin, blood vessels from the alveolar arteries grow into the papilla, and the papilla cells are transformed into pulp tissue. The cells are distinguished on the basis of their form and function: the odontoblast layer, fibroblasts, replacement cells, and defensive cells.
The main cell mass is made up of fibroblasts, while the peripheral boundary is occupied by odontoblasts. In addition, there are free-moving cells—lymphocytes, monocytes, and histiocytes— that act as defensive cells of normal connective tissue. The fibers and fibrils of the pulp tissue are connected in orderly states to the fibers of the periodontal ligament (desmodontium) at the apical root pulp.
The functions of pulp are to:
- Nourish the odontoblasts
- Replace destroyed odontoblasts
- Be indirectly involved in dentin formation
- Give warning of pain in response to mechanical, thermal, and chemical irritation
- Act as a defensive function via phagocyte systems
Pulp functions are performed better by young pulp tissue than by aging tissue. Functional capacity declines as the pulp cavity narrows, the vessel density decreases, and collagen fibers are embedded. Mineral deposits (pulp stones or denticles) and calcifications, chronic disease processes (eg, caries, infections), as well as careless, damaging dental procedures further limit this functional capacity.
The pulp can sustain reversible or even irreversible damage during preparation of crown stumps or cavities. Pulp irritation can arise, depending on the abrasive pressure applied, heat generated by grinding, or the use of chemical cleaning and filling materials. The best-case scenario is merely short-term, reversible damage to the odontoblast function, combined with inflammatory processes in the pulp that act as a stimulus to the synthesis of secondary dentin. This is exploited for therapeutic purposes to subsequently reach greater preparation depths (eg, for ceramic or composite resin crowns for young teeth).
Temperature increases due to abrasion heat of more than 8°C above 37°C will produce irreversible cell and tissue damage as a result of precipitation of protein. If impression material is too hot, there may be temperature peaks of 53°C in the pulp, which are enough to kill off the odontoblast layer, cause chronic inflammation, and devitalize the tooth. An added problem is that the tooth may remain symptom-free for months or even years after this kind of damage.