Eccentric Splints
Repositioning splints and distraction (decompression) splints may be described as types of "eccentric splint" (ie, out of centric relation).
The repositioning splint can be used to bring the mandible into an anterior position in order to bring a partially or totally displaced articular disc into its physiologic position and create a click-free and painless situation. The aim is to restore a normal condyle-disc relationship through this temporary anterior displacement of the mandible.
Anterior displacement of the maxilla of not more than 1.0 to 1.5 mm by the splint is therapeutically successful. In a case of disc dislocation, the connective tissue suspending the disc is stretched or damaged, making it difficult to securely fix the condyle-disc relationship in the new occlusal position. This means that a relapse (recurrence) can happen after completion of treatment even in favorable conditions.
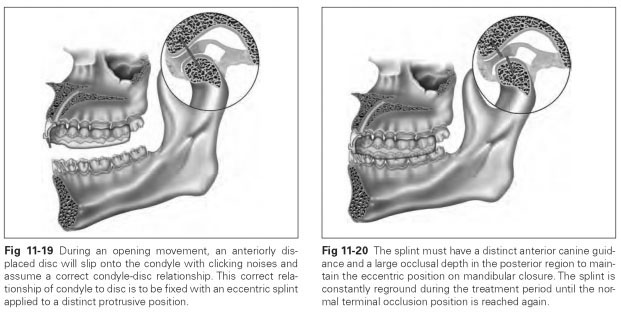
Repositioning splints are reground constantly during the wearing period to bring the mandible gradually out of the protrusive position back in a dorsal direction and the condyle back into its normal anatomical position (Fig 11-19). At the end of treatment, a stable occlusion must exist and anterior canine guidance must be either present or producible by prosthetic methods.
This method requires regular appointments to ensure that the occlusal contact relationships are not altered, eg, no posterior open bite develops. Once the acute symptoms have subsided, the treatment should be continued with stabilization splints. The physiologic condyle-disc relationship is usually restored more quickly with stabilization splints.
The repositioning splint must be worn continuously, even while eating. The wearing time extends to a minimum of 6 months, until the joint noises and symptoms have disappeared. To prevent a relapse, a retainer can be used to stabilize the therapeutic position.
The therapeutic position (in the case of a repositioned disc) must be measured and transferred to an articulator so that the splint can be fabricated in that position. A repositioning splint should be made for the maxilla because of the wearing mode, and the occlusal contacts should be worked into it. So that the new position is found and fixed without any problems, anterior canine guidance and a large occlusal depth must be created (Fig 11-20).
Repositioning splints are intended to ensure the centric mandibular position by means of uniform intercuspation where the teeth have numerous contacts with each other. Engagement in the contact pattern can thus be achieved without having to make any irreversible changes to the teeth.
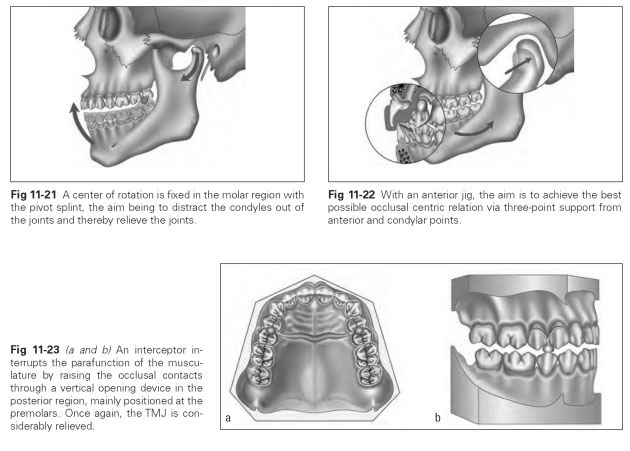
A distraction splint (pivot splint, decompression splint) is the treatment method used to eliminate disc displacement without reduction or to relieve compressed TMJs by creating an artificial premature contact in the molar region (Fig 11-21). The TMJ is actually relieved when the condyle is pushed out of the fossa on biting together on the premature contact in the molars. As the joint is relieved, the joint capsules, muscles, and ligaments are stretched. To create the artificial premature contact, 0.3- to 0.9-mm-thick tin foil can be inserted into the condylar housing of the articulator so that the occlusion is raised in the dorsal area
or the posterior teeth are blocked. The distraction splint is fabricated in this model position. The splint is worn as often as possible, until freedom from pain is achieved and unrestricted mouth opening is possible; this can take up to 6 months. The distraction splint with extreme distraction of 1 mm enables a displaced disc to be guided back, although with a risk of additional joint damage.
Partial splints can also be used to correct jaw relations.
The anterior jig offers incisal horizontal guidance to adjust the centric relation during prosthetic measures (Fig 11-22).
The interceptor is a clasp-retained palatal bar produced by model casting with bilateral ball-head or cylindric supports in the premolar region. It interrupts habitual parafunctions of the muscles of mastication by placing all the teeth out of contact (Fig 11-23).